Dental health is a crucial aspect of our overall well-being, directly influencing our ability to eat, speak, and interact confidently with others. Among the various dental solutions available today, dental implants stand out as a revolutionary advancement. This guide delves deep into the world of dental implants, exploring their history, benefits, types, procedure, aftercare, and how they compare to other tooth replacement options.
Whether you’re considering dental implants for yourself or simply curious about this modern marvel, this comprehensive guide aims to provide all the information you need.
A Brief History of Dental Implants
The concept of dental implants isn’t as modern as one might think. Ancient civilizations attempted rudimentary tooth replacements using materials like seashells and carved stones. However, the modern dental implant as we know it began to take shape in the mid-20th century.
In the 1950s, Dr. Per-Ingvar Brånemark, a Swedish orthopedic surgeon, made a groundbreaking discovery. He found that titanium could fuse with bone, a process he termed “osseointegration.” This discovery led to the development of the first successful dental implant. Over the decades, advancements in technology and materials have refined the procedure, making dental implants a highly effective and reliable solution for tooth replacement.
Understanding Dental Implants
What Are Dental Implants?
Dental implants are artificial tooth roots made of biocompatible materials like titanium. They are surgically placed into the jawbone, where they provide a sturdy foundation for a replacement tooth, bridge, or denture. The implant integrates with the bone over time, mimicking the function and appearance of natural teeth.
Components of a Dental Implant
- Implant Fixture: The implant fixture is the titanium post that is surgically placed into the jawbone. It acts as the root of the artificial tooth.
- Abutment: The abutment is a connector that is placed on top of the implant fixture. It holds and supports the replacement tooth.
- Crown: The crown is the visible part of the implant that resembles a natural tooth. It is custom-made to match the color and shape of the patient’s natural teeth.
Benefits of Dental Implants
1. Improved Appearance
Dental implants are designed to look, feel, and function like natural teeth. They blend seamlessly with the patient’s existing teeth, providing a natural and aesthetically pleasing appearance.
2. Enhanced Comfort
Unlike traditional dentures, dental implants are permanently fixed in place. This eliminates the discomfort and inconvenience associated with removable dentures, such as slipping and sore spots.
3. Better Oral Health
Dental implants do not require the alteration of adjacent teeth, as is necessary with traditional bridges. This helps preserve the natural tooth structure and maintain overall oral health.
4. Durability and Longevity
With proper care and maintenance, dental implants can last a lifetime. They are highly durable and can withstand the forces of chewing and biting.
5. Improved Speech and Eating
Dental implants restore the full function of the mouth, allowing patients to speak clearly and eat a variety of foods without restriction.
6. Bone Preservation
Implants help preserve the jawbone by stimulating bone growth through osseointegration. This prevents bone loss, a common issue with missing teeth.
Types of Dental Implants
1. Endosteal Implants
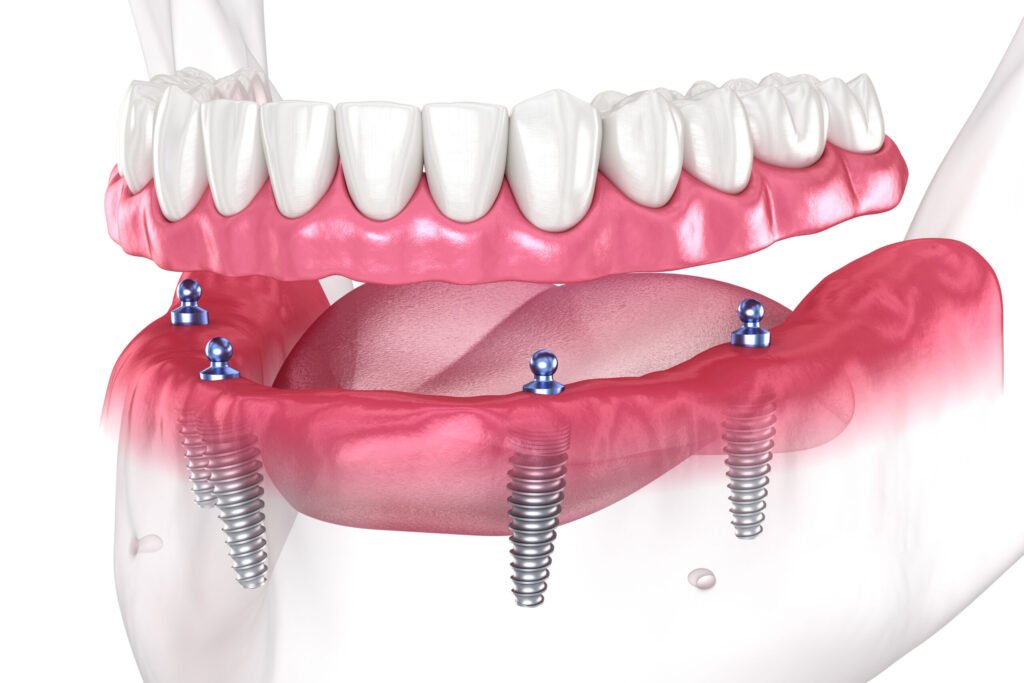
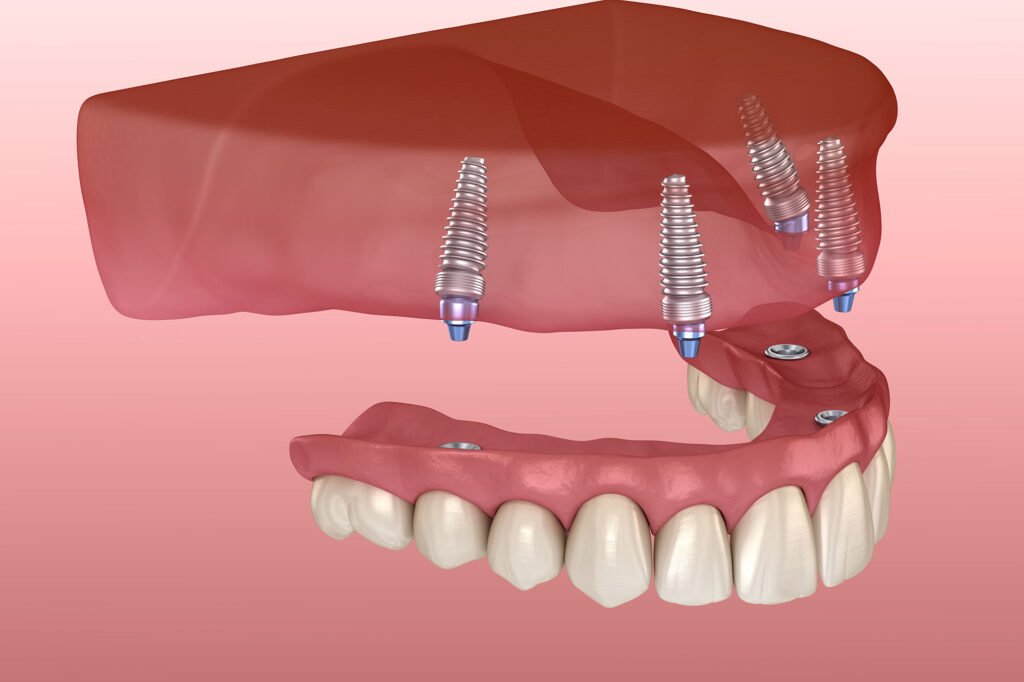
Endosteal implants are the most common type of dental implant. They are typically shaped like small screws and are placed directly into the jawbone. Once the surrounding gum tissue has healed, a second surgery is required to connect the abutment to the implant. Finally, the artificial tooth is attached to the abutment.
2. Subperiosteal Implants
Subperiosteal implants are used when there is not enough healthy jawbone to support endosteal implants. These implants are placed under the gum but on or above the jawbone. A metal framework is fitted onto the jawbone, and the artificial teeth are attached to the framework.
3. Zygomatic Implants
Zygomatic implants are used in cases of severe bone loss in the upper jaw. They are anchored in the cheekbone (zygomatic bone) rather than the jawbone. This type of implant requires specialized surgical expertise.
The Dental Implant Procedure
Initial Consultation and Assessment
The journey to getting dental implants begins with an initial consultation with a dental professional. During this visit, the dentist will:
- Review the patient’s medical and dental history.
- Conduct a thorough oral examination.
- Take X-rays and, in some cases, a CT scan to assess bone density and determine the optimal implant placement.
- Discuss the patient’s expectations and any concerns.
Treatment Planning
Based on the assessment, the dentist will develop a customized treatment plan. This plan outlines the steps involved in the implant process, including the number of implants needed, the type of implant, and any additional procedures, such as bone grafting or sinus lifts.
Surgical Placement of Implants
The surgical placement of dental implants typically involves the following steps:
- Anesthesia: Local anesthesia or sedation is administered to ensure the patient’s comfort during the procedure.
- Incision: An incision is made in the gum tissue to expose the jawbone.
- Drilling: A hole is drilled into the jawbone to create space for the implant.
- Implant Placement: The titanium implant is inserted into the prepared hole.
- Suturing: The gum tissue is stitched closed over the implant.
Osseointegration
After the implants are placed, a process called osseointegration occurs. This involves the fusion of the implant with the surrounding bone, creating a strong and stable foundation. Osseointegration typically takes several months, during which time the patient may receive a temporary restoration to maintain aesthetics and function.
Abutment Placement
Once osseointegration is complete, a minor surgical procedure is performed to attach the abutment to the implant. This procedure involves:
- Making a small incision to expose the implant.
- Attaching the abutment to the implant.
- Allowing the gum tissue to heal around the abutment.
Final Restoration
The final step in the dental implant process is the placement of the artificial tooth, bridge, or denture. This involves:
- Taking impressions of the patient’s mouth to create a custom-made restoration.
- Ensuring that the color, shape, and size of the restoration match the natural teeth.
- Attaching the restoration to the abutment, ensuring a secure and comfortable fit.
Aftercare and Maintenance
Proper aftercare and maintenance are essential to ensure the longevity and success of dental implants. Patients should:
- Practice good oral hygiene, including regular brushing, flossing, and rinsing with an antibacterial mouthwash.
- Attend regular dental check-ups and cleanings.
- Avoid chewing on hard objects, such as ice and hard candies, to prevent damage to the implants.
- Quit smoking, as it can negatively affect the healing process and increase the risk of implant failure.
- Follow the dentist’s post-operative care instructions, including dietary recommendations and any prescribed medications.
Comparing Dental Implants to Other Tooth Replacement Options
Dental Implants vs. Dental Bridges
- Longevity: Dental implants can last a lifetime, whereas dental bridges typically need replacement every 10-15 years.
- Oral Health: Implants do not require the alteration of adjacent teeth, preserving natural tooth structure. Bridges involve the modification of surrounding teeth to support the bridge.
- Bone Health: Implants stimulate bone growth and prevent bone loss, while bridges do not provide this benefit.
Dental Implants vs. Dentures
- Stability: Dental implants are securely fixed in place, eliminating the risk of slipping or shifting. Dentures can move and cause discomfort.
- Functionality: Implants restore full chewing and biting function, allowing patients to eat a wider variety of foods. Dentures may require dietary restrictions.
- Comfort: Implants feel more like natural teeth and do not cause sore spots or irritation. Dentures can cause discomfort and require regular adjustments.
Conclusion
Dental implants have revolutionized the field of dentistry, offering a permanent and reliable solution for tooth replacement. With their numerous benefits, including improved appearance, enhanced comfort, and better oral health, dental implants have become the preferred choice for many patients seeking to restore their smiles.
By understanding the history, components, procedure, and aftercare involved in dental implants, patients can make informed decisions and enjoy the life-changing benefits of this remarkable dental innovation. Whether you’re considering dental implants for yourself or a loved one, this ultimate guide serves as a comprehensive resource to help you navigate the journey to a healthier, more confident





